A 66Y old male patient came with c/o fever since 15 days
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning
Case discussion:
A 66Y old male patient resident of nalgonda came with chief complaints of fever since 15 days and pain in right iliac fossa since 10 days
Patient was apparently asymptomatic 8 months back then he developed pain in right hypochindrium , he went to a private hospital where he got his USG abdomen done and diagnosed with cholelithiasis for which symptomatic management was done
He developed fever since 15days which is high grade, intermitent associated with chills and rigors which got relieved on medication(DOLO 650mg TID) . It is associated with loss of appetite since 15 days
Then he developed Pain abdomen in right iliac fossa since 10 days, pricking type , radiating to epigastric and left hypochondriac region ,followed by shortness of breath(grade1) since 3 days.
No h/o vomitings, loose stools, orthopnea,weight loss,altered bowel habits
PAST HISTORY:
Not a k/c/o DM, HTN, asthma , epilepsy, CKD,CHD
S/P: perineal urethrostomy done 10 years as he developed complete stricture of urethra at private hospital in hyderabad.
H/O BPH symptoms (Poor urine stream, frequency, urgency) 2 months back for which he got treated with URIMAX-D
HABITS:
He was on mixed diet,loss of appetite since 15 days, bowel and bladder movements are regular, sleep is adequate ,ocassional alcoholic since 15 years but completely stopped 5 years back
FAMILY HISTORY: no similar complaints
GENERAL EXAMINATION: Patient is conscious, coherent , co operative
oriented to time , place and person,
moderately built and nourished
VITALS: BP- 110/70mmhg
pulse-78bpm
Temp-afebrile
RR-24cpm
Spo2-98% at room air
No pallor, icterus,cyanosis, clubbing, koilonychia, lymphadenopathy and pedal edema
SYSTEMIC EXAMINATION:
PER ABDOMEN:
O/E:
Abdomen is distended
Umbilicus is inverted
On palpation,it is soft and tenderness present in right iliac fossa , epigastric and left hypochondriac regions
Hepatomegaly is present(liver span-16cms)
Bowel sounds heard
CVS: s1 s2 heard, no murmurs
RS:
BAE present, normal vesicular breath sounds were heard, no added sounds.
CNS: higher mental functions-normal
Cranial nerves- intact
motor system-intact
Sensory system- intact
No cerebellar signs
INVESTIGATIONS:
HB - 11.5gm/dl,
TLC - 20000
PLT- 4.5lakh.
CUE- pus cells- 8 to 10, Rbc- bacteria present, albumin - plus 2,
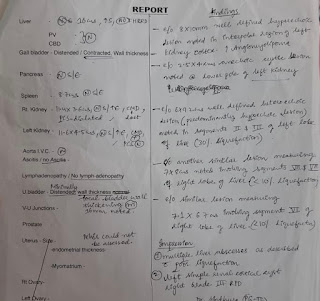
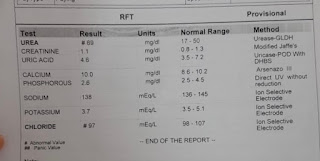
RFT- UREA- 69mg/DL, creatinine - 1.1mg/DL, NA - 138meq/l, k- 3.7, cl- 97,
LFT - TB - 1.62, DB - 1.00, ALP 804, ALBUMIN 2.5GM/DL,
PROVISIONAL DIAGNOSIS:
MULTIPLE LIVER ABSCESS
TREATMENT - INJ PIPTAZ 4.5gmiv tid,
INJ METRONIDAZOLE750mg IV tid,
INJ PAN 40mgiv OD,
IV FLUIDS,
TAB URIMAX-D OD.


















Comments
Post a Comment